Home > Research Hubs > Acellular / smart materials – 3D architecture > Case Studies
BioYarn: stitches for tendons using regenerative medicine
Surgical interventions to repair torn tendons aren’t always effective, and patients continue to experience significant pain and disability if the repair fails. Harnessing the power of regenerative medicine, using a novel synthetic material suture offers new hope to patients with this injury.
Tearing of the rotator cuff tendons affects around 25% of the population over the age of 60 and can result in significant pain and disability. Although management of these tears is often conservative, many patients undergo surgical interventions to attempt to generate a functional repair. Unfortunately, recent evidence has shown that 40% of repairs fail within 12 months irrespective of the surgical technique used, demonstrating the need for a new approach to tackle this problem.
Professor Andrew Carr and Professor Pierre-Alexis Mouthuy in Oxford are designing a synthetic material suture called BioYarn which mimics the natural environment required by cells to achieve a successful tendon repair. BioYarn utilises a technology called “electrospinning” which uses electrical charges to create aligned microfibres out of a polymer solution. These biomimetic fibres can then be assembled into a multifilament suture using established textile technologies. In vivo, human cells respond to this biomimetic structure by migrating into the material and growing new tissue. Over time, the suture degrades to harmless by-products, leaving only natural repaired tissue in its place.
In order to transition from laboratory experiments to clinical use, the Oxford team has scaled up the manufacturing process to a manufacturing chain capable of significantly higher output. Additionally, the manufacturing environment has transitioned to an ISO 7 controlled cleanroom environment. These quality standards are crucial for accelerating therapies to clinical use. At the same time, the team have also progressed preclinical testing which follows guidance from the ISO standards surrounding medical device design and development. This work further helps to evidence the safety and efficacy of BioYarn, while complying with regulatory requirements established to allow a first in human clinical study to be performed using BioYarn.
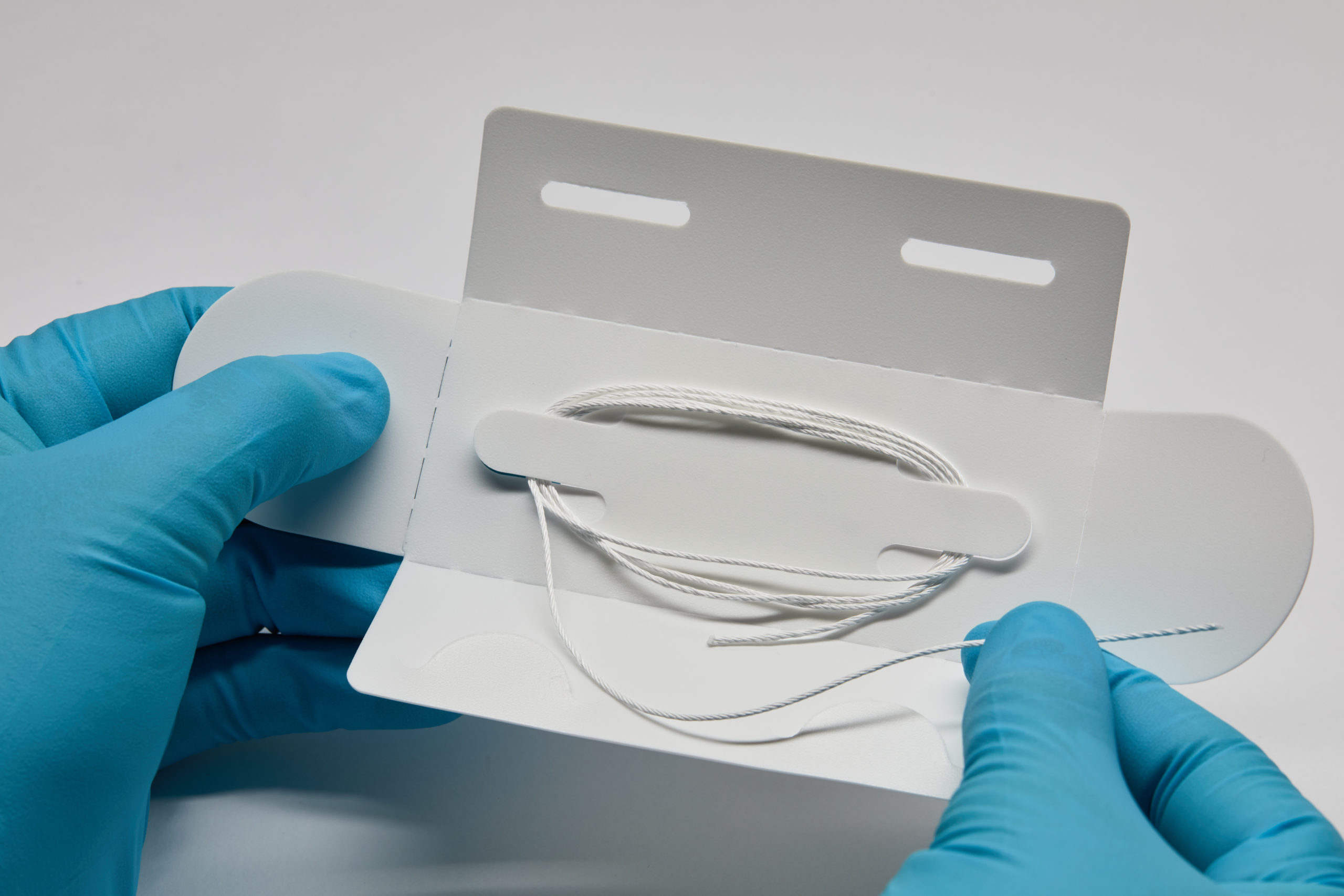
Image: BioYarn, a twisted electrospun suture.
Regenerating bone with nanoclay gels
Stem cell differentiation relies on key biochemical signals from the local environment surrounding them. This environment can be difficult to replicate when developing therapies using stem cells, as conventional biomaterials struggle to retain these biochemical signals. Nanoclay gels offer an exciting solution to this problem, as they can form gels that bind such biochemical signals to create environments favourable for stem cells to colonise.
Dr Jon Dawson at the University of Southampton is working on developing injectable nanoclay gels to activate stem cells for bone regeneration. Stem cells can cure a variety of conditions by regenerating tissue. They are activated by powerful biochemical molecules from within their local microenvironment. Localising and retaining these bioactive molecules close to a healing site is key to the safety and efficacy of regenerative medicine applications. However, conventional biomaterials are often poor at retaining these molecules at the site of injury, and the molecules that stimulate the cells usually diffuse away.
The team have developed a nanoclay gel that can support stem cell growth and colonization. They have characterized the cellular response to nanoclay, including how it promotes the recruitment and entry of stem cells. The team also studied the potential effects of nanoclay degradation products on stem cell differentiation. They have shown that nanoclay gels can promote the entry of stem cells to a site of injury and promote remodelling, which is instrumental for bone regeneration. They also showed that the implanted nanoclay gels are degraded by cells and safely processed by the body. These results are now being used to support a submission to the FDA requesting a designated classification for this technology.
Intriguingly, the work has also opened new possibilities and collaborations for understanding the interactions of immune cells within the stem cell microenvironment. For example, the team showed that the early inflammatory response to the nanoclay actually promoted the subsequent regenerative action. The team in Southampton are now working with researchers in Japan on a new £600k three-year collaborative project to explore the early immune response to nanoclays as a springboard for bone repair processes.
A little goes a long way: ultra-low dose growth factor treatments for bone repair
Sometimes broken bones do not heal even with the best surgical or non-surgical treatments. These fractures can be treated successfully with growth factors, but it is expensive and comes with serious side effects because of the high doses of growth factors. New techniques to deliver growth factor treatments at ultra-low doses can help address this problem and help safely heal previously untreatable fractures.
Professor Manuel Salmeron-Sanchez at the University of Glasgow has developed a type of polymer coating called PEA (poly ethyl acrylate) that spontaneously organises key proteins in the extracellular matrix of bone tissue into a network that stimulates signalling of the key growth factor, BMP-2. This in turn allows the researchers to use ultra-low doses of BMP-2, which avoid the serious side effects such as such as ectopic bone formation and high risk of cancer that are sometimes seen with BMP-2 treatment.
The team used ceramic granules coated with PEA to successfully treat several bone defects in pre-clinical models. The team also first demonstrated efficacy in a small animal model where they demonstrated bone regeneration using 100 times less BMP-2 compared to levels typically used in this model. In parallel, researchers had the opportunity to treat a veterinary patient, Eva, a 2 years-old dog who was run over by a car which shattered the bones in her leg. Though her fractured humerus was fixed with conventional plates, a subsequent infection of the fracture led to a defect where the broken bones did not heal correctly. They successfully treated Eva’s fracture with their PEA-coated granules.
Since then, the team have successfully treated another twelve veterinary cases (dogs and cats) with different challenging fractures. The researchers are currently testing a large animal model with the technology in collaboration with researchers at the University of Nottingham, with promising early results. The team is currently working in partnership with a company in Spain (Histocell) to move the manufacturing of the polymer coating to standardized quality conditions to facilitate the regulatory approvals needed for progressing this exciting research into clinical trials.
Case studies written by Dr Buddhini Samarasinghe, Science Writer, MRC